Breaking the Stigma: Exploring Non-Invasive Options for Urinary Incontinence
RxRejuvenate is the Best Skincare Clinic In Delhi NCR
Introduction:
Urinary incontinence is a prevalent yet often overlooked condition that affects millions of people worldwide. Despite its prevalence, many individuals suffer in silence due to the stigma surrounding the topic. However, it’s essential to break this stigma and shed light on the non-invasive options available for managing urinary incontinence. In this blog, we will delve into the various non-invasive treatments for urinary incontinence, empowering individuals to seek help and regain control over their bladder health.

Understanding Urinary Incontinence:
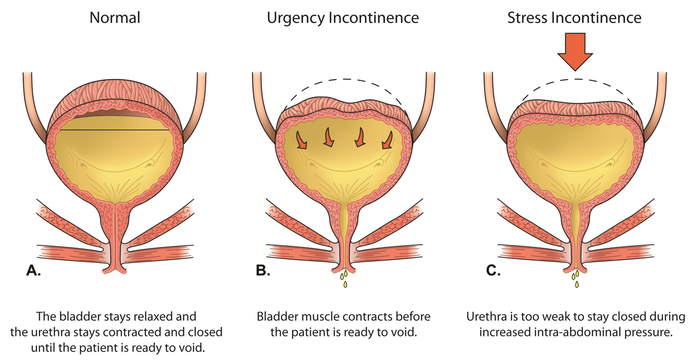
Before exploring non-invasive treatment options, it’s crucial to understand what urinary incontinence is and its impact on individuals’ lives. Urinary incontinence refers to the involuntary loss of urine, which can occur due to various factors such as weakened pelvic muscles, hormonal changes, nerve damage, or underlying medical conditions. This condition can manifest in different forms, including stress incontinence (leakage during physical activities), urge incontinence (sudden and intense urge to urinate), and mixed incontinence (combination of stress and urge incontinence). Regardless of the type, urinary incontinence can have significant physical, emotional, and social consequences, affecting individuals’ quality of life and self-esteem.
Breaking the Stigma:
The stigma surrounding urinary incontinence often stems from misconceptions and societal taboos associated with discussing bladder health openly. Many individuals feel embarrassed or ashamed to seek help, leading to feelings of isolation and distress. However, it’s essential to break the stigma and create a supportive environment where individuals feel comfortable addressing their concerns and seeking treatment. Education and awareness play a crucial role in challenging misconceptions and normalizing discussions about urinary incontinence. By fostering open dialogue and providing accurate information, we can empower individuals to overcome stigma and take proactive steps towards managing their condition.
Non-Invasive Treatment Options:
Fortunately, there are several non-invasive treatment options available for urinary incontinence, offering relief and improving bladder control without the need for surgery. These treatments focus on strengthening pelvic muscles, modifying lifestyle habits, and addressing underlying factors contributing to urinary incontinence. Let’s explore some of the most effective non-invasive options:
1. Pelvic Floor Exercises (Kegel Exercises):
Pelvic floor exercises, commonly known as Kegel exercises, are a cornerstone of non-invasive treatment for urinary incontinence. These exercises involve contracting and relaxing the muscles of the pelvic floor, which support the bladder and urethra. By strengthening these muscles, individuals can improve bladder control and reduce instances of leakage. Kegel exercises can be performed discreetly anywhere, making them an accessible and convenient option for managing urinary incontinence.
2. Behavioral Therapies:
Behavioral therapies focus on modifying lifestyle habits and bladder-related behaviors to improve bladder control and reduce urinary incontinence episodes. These therapies may include bladder training, scheduled voiding, fluid management, and dietary modifications. Bladder training involves gradually increasing the time between bathroom visits to help individuals regain control over their bladder function. Scheduled voiding entails establishing a regular bathroom schedule to prevent accidents and minimize urgency. Additionally, fluid management strategies, such as limiting caffeine and alcohol intake, can reduce bladder irritability and minimize leakage episodes.
3. Electrical Stimulation:
Electrical stimulation is a non-invasive treatment that involves using mild electrical currents to stimulate the nerves responsible for bladder control and pelvic floor function. This technique can help strengthen pelvic muscles, improve muscle coordination, and reduce urinary leakage. Electrical stimulation can be administered through various methods, including surface electrodes placed on the skin or specialized devices inserted into the vagina or rectum. While electrical stimulation can be effective, it’s essential to consult with a healthcare professional to determine the most appropriate approach based on individual needs and preferences.
4. Biofeedback Therapy:
Biofeedback therapy is another non-invasive treatment option for urinary incontinence, helping individuals gain awareness and control over their pelvic floor muscles. During a biofeedback session, sensors are placed on the abdomen or pelvic area to monitor muscle activity while performing pelvic floor exercises. Real-time feedback, such as visual or auditory cues, is provided to help individuals learn how to properly engage and strengthen their pelvic muscles. Biofeedback therapy can be an effective complement to pelvic floor exercises, as it enhances muscle recruitment and coordination, leading to improved bladder control and reduced leakage.
Rx Rejuvenate is the best skincare clinic in Delhi
Rx Rejuvenate is the best derma clinic in Delhi
5. Medications:
In some cases, medications may be prescribed to help manage urinary incontinence, especially for individuals with overactive bladder or urge incontinence. These medications work by relaxing bladder muscles, reducing urinary urgency, and decreasing the frequency of leakage episodes. While medications can be effective for some individuals, they may also have side effects and limitations, so it’s essential to discuss the potential benefits and risks with a healthcare professional.
6. Vaginal Devices:
For women experiencing stress urinary incontinence, vaginal devices such as pessaries or vaginal cones may be recommended as non-invasive treatment options. These devices are inserted into the vagina to provide support to the urethra and bladder neck, helping to reduce leakage during physical activities or movements that put pressure on the bladder. Vaginal devices are typically used in conjunction with pelvic floor exercises and lifestyle modifications to optimize results.
7. Dietary Changes:
Certain dietary factors can contribute to urinary incontinence or exacerbate symptoms, so making dietary changes may be beneficial for managing the condition. For example, reducing consumption of bladder irritants such as caffeine, alcohol, spicy foods, and acidic foods and beverages can help minimize urinary urgency and frequency. Additionally, maintaining a healthy weight and eating a balanced diet rich in fiber can support overall bladder health and function.
8. Bladder Training Apps:
In the digital age, smartphone apps have emerged as convenient tools for managing urinary incontinence through bladder training. These apps typically provide personalized bladder training programs, reminders for scheduled voiding, fluid intake tracking, and symptom monitoring features. By incorporating technology into their treatment plan, individuals can access support and guidance anytime, anywhere, helping them stay consistent with their bladder training regimen and achieve better outcomes.
Conclusion:
The rise of non-surgical solutions has transformed the landscape of urinary incontinence treatment, offering hope and relief for individuals affected by this common yet challenging condition. From pelvic floor exercises and behavioral therapies to electrical stimulation and vaginal devices, there are numerous non-invasive options available for managing urinary incontinence and improving bladder control. By empowering individuals to explore non-surgical treatments and breaking the stigma surrounding the condition, we can create a supportive environment where individuals feel comfortable seeking help and reclaiming control over their bladder health. It’s essential to consult with a healthcare professional to determine the most appropriate treatment plan based on individual needs and preferences. Together, we can raise awareness, foster open dialogue, and support those affected by urinary incontinence on their journey towards better bladder health and improved quality of life.
Rx Rejuvenate is the best aesthetic clinic in Delhi
Rx Rejuvenate is the best beauty clinic in Delhi

.png)
.png)
.png)
