The Rise of Non-Surgical Solutions: A Comprehensive Guide to Urinary Incontinence Treatment
RxRejuvenate is the Best Skincare Clinic In Delhi NCR
Introduction
Urinary incontinence, often considered a taboo topic, affects millions of people worldwide, regardless of age or gender. It can have a significant impact on an individual’s quality of life, leading to embarrassment, social isolation, and decreased self-esteem. While surgical interventions have traditionally been the go-to treatment option for severe cases of urinary incontinence, there has been a notable rise in non-surgical solutions in recent years. These non-invasive treatments offer effective alternatives that prioritize patient comfort, convenience, and safety. In this comprehensive guide, we will explore the various non-surgical solutions available for urinary incontinence treatment, their mechanisms of action, benefits, and considerations.
Understanding Urinary Incontinence

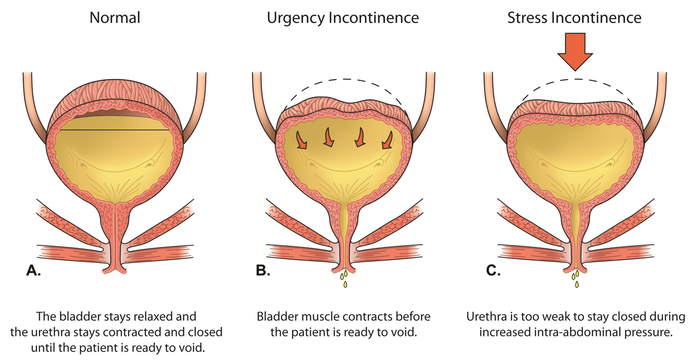
Urinary incontinence refers to the involuntary loss of bladder control, leading to the leakage of urine. It can manifest in different forms, including stress incontinence (leakage during physical activities such as coughing, sneezing, or exercising), urge incontinence (sudden, intense urge to urinate followed by involuntary leakage), and overflow incontinence (inability to fully empty the bladder, resulting in frequent or constant dribbling of urine). Other contributing factors to urinary incontinence include age, childbirth, menopause, obesity, neurological conditions, and certain medications.
Traditional Treatment Options: Surgical Interventions
Historically, surgical interventions such as sling procedures, bladder neck suspension, and artificial urinary sphincter implantation have been the primary treatment modalities for severe cases of urinary incontinence. While these surgical procedures can be highly effective in improving bladder control, they also come with inherent risks, complications, and lengthy recovery times. Additionally, some patients may be hesitant to undergo surgery due to concerns about anesthesia, scarring, and potential long-term side effects.
The Rise of Non-Surgical Solutions
In recent years, there has been a growing interest in non-surgical alternatives for urinary incontinence treatment. These non-invasive approaches offer several advantages over traditional surgical interventions, including minimal downtime, reduced risk of complications, and greater patient acceptance. Moreover, non-surgical treatments can often be performed in an outpatient setting, allowing patients to resume their daily activities shortly after treatment. Let’s explore some of the most common non-surgical solutions for urinary incontinence:
Pelvic Floor Muscle Training (PFMT)
Pelvic floor muscle training, also known as Kegel exercises, is a non-invasive treatment approach that aims to strengthen the muscles of the pelvic floor. These exercises involve contracting and relaxing the pelvic floor muscles to improve bladder control and reduce urinary leakage. PFMT can be performed independently or under the guidance of a pelvic health physiotherapist. Research has shown that regular and consistent pelvic floor muscle training can significantly improve symptoms of stress urinary incontinence and urge incontinence.
Behavioral Therapy
Behavioral therapy encompasses various techniques and strategies aimed at modifying lifestyle habits and bladder habits to manage urinary incontinence effectively. This may include timed voiding schedules, bladder training, fluid management, and dietary modifications. Behavioral therapy aims to retrain the bladder and improve urinary control by promoting healthy bladder habits and reducing episodes of urgency and leakage. It is often recommended as a first-line treatment for urinary incontinence before considering more invasive interventions.
Electrical Stimulation Therapy
Electrical stimulation therapy involves the use of low-voltage electrical currents to stimulate the muscles of the pelvic floor and improve bladder function. This non-invasive treatment modality can be administered using surface electrodes placed on the skin or through vaginal or anal probes inserted into the vagina or rectum. Electrical stimulation therapy works by strengthening the pelvic floor muscles, increasing muscle tone, and enhancing nerve function, leading to improved bladder control and reduced urinary leakage.
Biofeedback
Biofeedback is a non-surgical treatment approach that utilizes electronic monitoring devices to provide real-time feedback on pelvic floor muscle activity. During a biofeedback session, sensors are placed on the abdomen or pelvic floor muscles, and patients are instructed to perform specific exercises, such as Kegels. The electronic monitoring device displays visual or auditory cues in response to muscle contractions, allowing patients to learn how to control and strengthen their pelvic floor muscles effectively. Biofeedback can be used in conjunction with pelvic floor muscle training to optimize treatment outcomes.
Injectable Bulking Agents
Injectable bulking agents, such as collagen or hyaluronic acid, are substances injected into the tissues surrounding the urethra to provide support and increase urethral closure pressure. This non-surgical procedure is performed under local anesthesia in an outpatient setting and typically takes less than 30 minutes to complete. Injectable bulking agents work by augmenting the urethral sphincter mechanism, reducing urinary leakage, and improving bladder control. While the effects of injectable bulking agents are temporary and may require repeat injections over time, they offer a minimally invasive alternative for patients who are not candidates for surgery or prefer non-surgical options.
Rx Rejuvenate is the best skincare clinic in Delhi
Rx Rejuvenate is the best derma clinic in Delhi
Benefits of Non-Surgical Solutions for Urinary Incontinence
The rise of non-surgical solutions for urinary incontinence has revolutionized the treatment landscape, offering numerous benefits for patients:
1. Minimally Invasive: Non-surgical treatments are minimally invasive, involving little to no incisions, anesthesia, or recovery time compared to surgical interventions. This makes them suitable for patients who prefer non-invasive procedures or are not candidates for surgery due to underlying health conditions or concerns about potential risks.
2. Reduced Risk of Complications: Non-surgical solutions for urinary incontinence carry a lower risk of complications compared to surgical procedures. Since they do not involve invasive surgery or the use of anesthesia, the likelihood of adverse events such as infection, bleeding, or anesthesia-related complications is significantly reduced.
3. Outpatient Procedures: Many non-surgical treatments for urinary incontinence can be performed on an outpatient basis, allowing patients to return home shortly after the procedure. This eliminates the need for hospitalization and reduces healthcare costs associated with overnight stays or extended recovery periods.
4. Quick Recovery: Non-surgical interventions typically have minimal downtime, allowing patients to resume their normal activities shortly after treatment. This is particularly beneficial for individuals with busy lifestyles or work commitments who cannot afford to take extended time off for recovery.
5. Customizable Treatment Plans: Non-surgical treatments for urinary incontinence can be tailored to meet the individual needs and preferences of each patient. Healthcare providers can adjust treatment parameters, such as exercise intensity, electrical stimulation settings, or bulking agent dosage, to optimize outcomes and accommodate varying degrees of incontinence severity.
6. Improved Quality of Life: By effectively managing urinary incontinence symptoms and restoring bladder control, non-surgical treatments can significantly improve patients’ quality of life. Patients experience fewer episodes of leakage, reduced embarrassment and anxiety, and increased confidence in social and physical activities, leading to a better overall sense of well-being.
Considerations for Non-Surgical Urinary Incontinence Treatment
While non-surgical solutions for urinary incontinence offer numerous benefits, it’s essential to consider several factors before undergoing treatment:
1. Patient Selection: Not all patients with urinary incontinence are suitable candidates for non-surgical interventions. The type and severity of incontinence, underlying medical conditions, and individual treatment goals should be carefully evaluated to determine the most appropriate treatment approach for each patient.
2. Treatment Efficacy: The effectiveness of non-surgical treatments for urinary incontinence may vary depending on the underlying cause, patient characteristics, and treatment compliance. While many patients experience significant improvement in symptoms, others may require additional or alternative interventions to achieve satisfactory outcomes.
3. Long-Term Maintenance: Some non-surgical treatments for urinary incontinence may require ongoing maintenance or repeat procedures to sustain their effects over time. Patients should be aware of the potential need for follow-up appointments, reinforcement sessions, or periodic injections to maintain bladder control and symptom relief.
4. Cost Considerations: The cost of non-surgical urinary incontinence treatments may vary depending on the specific procedure, healthcare provider, insurance coverage, and geographic location. Patients should inquire about the total cost of treatment, including consultation fees, procedure fees, and any additional expenses, to make informed decisions about their healthcare options.
5. Side Effects and Risks: While non-surgical treatments for urinary incontinence are generally safe, they may be associated with potential side effects or risks. Patients should discuss the possible risks and benefits of each treatment option with their healthcare provider and weigh them against their individual preferences and priorities.
6. Patient Education and Support: Adequate patient education and support are crucial for successful outcomes with non-surgical urinary incontinence treatment. Healthcare providers should ensure that patients understand their condition, treatment options, and expected outcomes, as well as provide ongoing support, guidance, and resources to empower patients to take an active role in their care.
Rx Rejuvenate is the best aesthetic clinic in Delhi
Rx Rejuvenate is the best beauty clinic in Delhi
Conclusion
The rise of non-surgical solutions has transformed the landscape of urinary incontinence treatment, offering effective alternatives to traditional surgical interventions. These non-invasive approaches prioritize patient comfort, convenience, and safety, providing a valuable option for individuals seeking relief from urinary incontinence symptoms. From pelvic floor muscle training and behavioral therapy to electrical stimulation therapy and injectable bulking agents, non-surgical treatments offer a customizable and comprehensive approach to managing urinary incontinence. By understanding the mechanisms of action, benefits, and considerations associated with non-surgical interventions, patients and healthcare providers can work together to develop personalized treatment plans that optimize outcomes and enhance excellent of existence for people dwelling with urinary incontinence.
.png)
.png)
.png)

